Dysplastic Nevi - Atypical Moles
The presence of dysplastic nevi is associated with an increased risk of melanoma, although many of these moles remain benign throughout a person's life. For individuals with numerous dysplastic nevi or those with a personal or family history of melanoma, regular dermatological assessments are important. Dermatologists utilize dermoscopy, a method involving a specialized magnification tool, to examine these moles more closely for any alarming changes. Sometimes, a biopsy may be needed to rule out cancer.
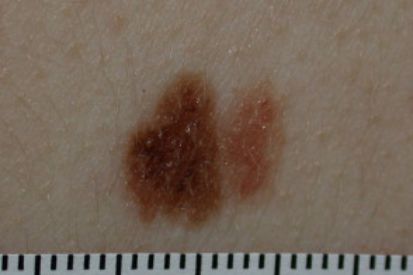
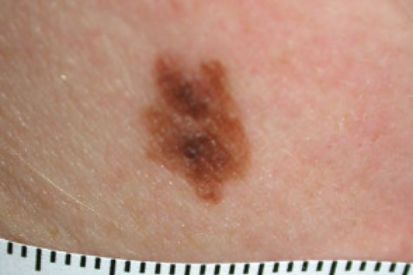
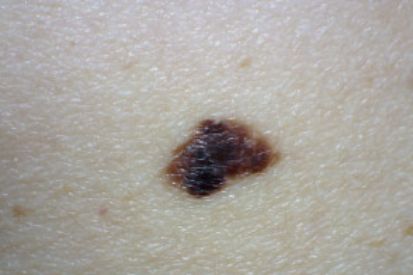
Examples of Dysplastic Nevi


What are the Symptoms of Dysplastic Nevi?
- Atypical moles are a size that exceeds that of common moles.
- These moles often exhibit a range of colors, including tan, brown, and red, creating an uneven or variegated appearance.
- The shape is irregular, featuring indistinct borders.
- They may appear either flat or slightly raised on the skin's surface, adding to their atypical nature.
- Dysplastic nevi are known for their potential to change over time. These changes can be alterations in size, color, or overall shape.
Causes of Dysplastic Nevi
- A family history of dysplastic nevi or melanoma indicates genetic predisposition.
- Exposure to UV radiation.
- Fair-skinned individuals with more moles are susceptible.
How to Prevent Dysplastic Nevi
- Sun Protection Measures: Wear protective clothing, including hats and long sleeves and use broad-spectrum sunscreen with a high SPF. Seek shade during peak sunlight hours between 10 a.m. and 4 p.m.
- Regular Skin Monitoring: Perform regular at-home self-exams of the skin and moles. Notify your dermatologist provider right away if you notice any unusual or evolving moles. It is also important to schedule an annual total body skin exam with one of our trusted providers.
- Awareness of Risk Factors: Individuals with a family history of dysplastic nevi or melanoma should be particularly vigilant, as they are at higher risk.
- Avoid Tanning Beds: Steer clear of tanning beds to reduce the risk of dysplastic nevi development.
FAQs for Dysplastic Nevi
Dysplastic nevi are not cancerous, but they can be considered precancerous. These moles have irregular features under the microscope and can appear larger, with uneven borders and varied colors compared to common moles. While most dysplastic nevi do not develop into melanoma, the presence of multiple dysplastic nevi is a marker of increased risk for melanoma. This means individuals with many dysplastic nevi should be more vigilant in monitoring their skin and regularly visiting a dermatologist for skin checks.
The risk of dysplastic nevi developing into melanoma is higher if there is a family history of melanoma or if the individual has numerous dysplastic nevi. However, not all dysplastic nevi will turn into cancer. Regular skin examinations and protective measures against UV exposure are crucial steps for those with dysplastic nevi to manage their risk effectively. Early detection and monitoring are key to preventing the progression from dysplastic nevi to melanoma.
Dysplastic nevi are diagnosed primarily through a thorough skin examination by a dermatologist. During the examination, the dermatologist looks for moles with atypical features such as irregular borders, varied colors, and larger size. If a mole appears suspicious, a biopsy may be performed, where a small sample of the mole is removed and examined under a microscope to assess its cellular structure. This histopathological analysis helps determine whether the mole is dysplastic and to what degree.
Once dysplastic nevi are diagnosed, regular monitoring is essential. Individuals with dysplastic nevi should undergo routine skin checks, typically every six to twelve months, depending on the number and severity of the nevi and their personal and family history of skin cancer. Self-examinations between professional check-ups are also important, where individuals should look for changes in the size, shape, color, or texture of their moles. Dermatoscopy, a non-invasive imaging technique, can also be used by dermatologists to monitor changes over time, providing a more detailed view of the moles. Early detection and consistent monitoring are crucial in managing the potential risk of dysplastic nevi progressing to melanoma.
Yes, dysplastic nevi can turn into melanoma, but it is not very common. Dysplastic nevi are considered to be at a higher risk for developing into melanoma compared to regular moles. The risk is particularly elevated in individuals who have a significant number of dysplastic nevi or a family history of melanoma. However, it is important to note that the majority of dysplastic nevi do not become cancerous. Instead, they serve as markers indicating an increased overall risk for developing melanoma.
To mitigate this risk, it is crucial for individuals with dysplastic nevi to engage in regular skin monitoring and protective measures. This includes routine dermatological check-ups, self-examinations, and adopting sun-safe behaviors, such as using sunscreen and wearing protective clothing. Early detection of any changes in dysplastic nevi can lead to prompt intervention, reducing the likelihood of progression to melanoma. Consistent monitoring and proactive management are key strategies in effectively addressing the potential risks associated with dysplastic nevi.
Yes, dysplastic nevi can develop anywhere on the body. They are most commonly found on sun-exposed areas such as the back, chest, and limbs, but they can also appear on less sun-exposed areas, including the scalp, buttocks, and breasts. Dysplastic nevi are irregular moles that may vary in size, shape, and color, making them distinct from common moles. Their occurrence is not limited to specific regions of the body, reflecting their potential to appear wherever melanocytes (the cells that produce pigment) are present.
The distribution of dysplastic nevi can be influenced by genetic factors and sun exposure. Individuals with numerous dysplastic nevi or a family history of such moles are more likely to have them appear in various locations across their body. Regardless of where they develop, it is important to monitor dysplastic nevi for any changes, as they can be an indicator of increased risk for melanoma. Regular skin examinations by a dermatologist and self-checks are crucial for early detection and management.
A total body skin exam by a dermatologist is crucial for early detection and prevention of skin cancer, including melanoma, basal cell carcinoma, and squamous cell carcinoma. Dermatologists are trained to recognize subtle changes in skin lesions that may indicate malignancy. During a comprehensive skin exam, the dermatologist can identify suspicious moles or growths that a person might overlook. Early detection of skin cancer significantly increases the chances of successful treatment and can prevent the cancer from spreading to other parts of the body, thereby reducing morbidity and mortality associated with advanced skin cancer.
Moreover, a total body skin exam is essential for individuals with a history of skin cancer, numerous moles, dysplastic nevi, or a family history of melanoma. These individuals are at a higher risk and require more vigilant monitoring. Dermatologists can provide personalized advice on sun protection and skin care, educate patients on how to perform self-examinations, and schedule regular follow-ups to monitor any changes over time. This proactive approach not only helps in catching potential skin cancers early but also in managing other dermatological conditions that might otherwise go unnoticed.
From Our QualDerm Family of Providers: Total Body Skin Exams
How to Treat Dysplastic Nevi
- Surveillance and Monitoring: One of our dermatologists will closely monitor dysplastic nevi due to their potential to transform into melanoma. Regular at-home self-exams are key – make sure to notify your dermatologist of any unusual or evolving moles. It is also important to schedule regular Total Body Skin Exams at one of our locations.
- Surgical Removal: If dysplastic nevi exhibits concerning features or irregularities during our providers’ evaluations, your dermatologist may recommend an excisional biopsy or complete removal.
- Reducing Malignancy Risk: Excisional biopsy aims to reduce the risk of potential malignancy by removing atypical moles.
- Regular Follow-ups: Individuals with a history of dysplastic nevi or a family history of melanoma should maintain regular visits with one of our skincare experts.
- Optimal Skin Health: While not all dysplastic nevi require treatment, their careful monitoring is crucial for optimal skin health and cancer prevention.
Featured Blogs

- Skin Cancer
- General Dermatology
- Skin Exams
Navigating the landscape of Total Body Skin Exams: Uncover the comprehensive process, understand why it matters for skin health, and gain insights into what to expect during these essential dermatological examinations.
Read More
- General Dermatology
- Skin Exams
- Chronic Skin Conditions
Explore our comprehensive guide to gain insights into accurate diagnosis and expert care for chronic skin conditions.
Read More
- Skin Cancer
- Skin Exams
In this blog, we’re covering what you need to know about five dangerous skin cancers, including basal cell carcinoma (BCC), squamous cell carcinoma (SCC), malignant melanoma, merkel cell carcinoma, and kaposi sarcoma.
Read MoreFeatured Products for Sun Protection

EltaMD UV Clear SPF 46 original
Oil-free EltaMD UV Clear helps calm and protect sensitive skin types prone to discoloration and breakouts associated to acne and rosacea. It contains niacinamide (vitamin B3), hyaluronic acid and lactic acid, ingredients that promote the appearance of healthy-looking skin. Very lightweight and silky, it may be worn with makeup or alone. Choose from tinted and untinted formulas for use every day. 1.7 oz / 48 g

SkinMedica Total Defense & Repair Broad Spectrum Sunscreen
Revolutionary non-tinted superscreen goes beyond UV protection to defend against harmful infrared rays while supporting the skin’s ability to restore itself. Appropriate for all skin types. 65 g / 2.3 oz


